Understanding Systemic Lupus Erythematosus (SLE)
- Isabelle Amigues
- Feb 10, 2023
- 4 min read
Updated: May 30, 2023
Have I told you how optimistic I am for patients with rheumatologic conditions? Well, I truly am! But I wasn’t this way for every rheumatologic conditions until recently.
Let me tell you about a diagnosis that has been making the headlines recently (Selena Gomez anyone): Systemic Lupus Erythematosus or SLE. When I started rheumatology back in the late 90’s (I started early, don’t calculate my age will you!). Anyway, when I started rheumatology, we were discovering drugs like remicade and humira (anti-TNF agents). We finally had something powerful to put our patients with Rheumatoid arthritis, Ankylosing spondylitis or psoriatic arthritis into disease remission. But one diagnosis continued to scare me for quite sometimes: Lupus. Indeed, while most of our patients were finally having some hope, it was clear that these newer medications did not do much for our patients with SLE. These patients felt like ticking bomb. One day they looked wonderful, the next they had a stroke or their kidneys were failing or they became suddenly short of breath with fluid built up in their lungs and hearts.
To face my fears, I decided to cross the Atlantic and move to the US to do some research with top Lupus specialist at Cornel University in New York city. I learnt a LOT! One of my proudest studies is one that looked at SLE patients and their serologies. We found that we could predict flares of their SLE by following their serologies. How cool is that to prevent a ticking bomb? But the best only appeared later, during my second rheumatology fellowship, this one at Columbia University in New York city. We finally had one, and soon after two new FDA approved treatments for SLE! So not only we are learning more and more about SLE every day, but we also now have more treatments for this condition. I am not afraid anymore and I can tell you that patients with SLE should be Hopeful!
In this blog post, I will discuss what SLE is, how it is diagnosed and treated, and why individuals should not be afraid when researching SLE online. And, of course, why you need a wonderful rheumatologist in your life (did I mention UnabridgedMD in Rheumatology is currently open to new patients?)
What is SLE?
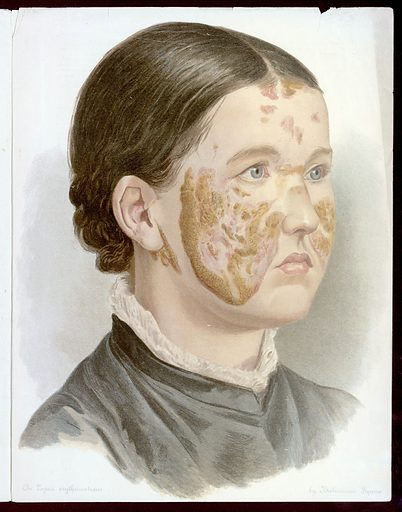
Systemic lupus erythematosus (SLE) is an autoimmune disorder in which the immune system mistakenly attacks healthy tissues instead of invading pathogens or foreign particles. This results in inflammation of various organs throughout the body such as the skin (example of Malar rash in the attached picture), joints, heart, lungs, kidneys, brain, and more. Symptoms of SLE vary greatly from person to person but may include joint pain/swelling; fatigue; fever; rashes; hair loss; chest pain; mouth sores; headaches; confusion/memory problems; seizures or strokes; organ failure; and more. Diagnosis of SLE usually requires that at least four specific criteria are met according to official diagnostic guidelines set by the American College of Rheumatology. Interestingly, due to its complexity and varying symptoms, it can be quite challenging to diagnose. From my own experience: I can either be consulted for patients with close to no symptoms (fatigue, maybe) and a positive ANA who do NOT have SLE, while some other patients may have gone years without having been seen by any rheumatologists and present to me with major organs involvement (kidney inflammation, stroke, inflammation of the heart etc..). We, rheumatologists, need to educate a lot more our colleagues so that patients with SLE are diagnosed early to prevent any damage to their organs.
How Is SLE Treated?
Treatment for SLE depends on the individual’s symptoms and other factors like age and overall health. Generally speaking, treatment involves medications such as non-steroidal anti-inflammatory drugs (NSAIDs); antimalarial drugs like hydroxychloroquine (plaquenil) or quinacrine in mild forms an immunosuppressants like azathioprine, cellcept or cyclophosphamide (Cytoxan); biologics like belimumab (Benlysta) or anifrolumab (Saphnelo); and as little as possible steroids. Many people with milder forms of SLE take only hydroxychloroquine while those with more severe forms may require any combination of these medications depending on their unique needs. There is a lot of hope for patients with SLE now that research has taken off and we are expecting to see a lot more treatments for this indication in the very near future.
Finally, there is enough scientific data to support lifestyle modifications. Yes, stress can cause flares and getting enough rest/sleep each night, avoiding overexertion during physical activities/exercise routines. We will also recommend to avoid direct sunlight whenever possible as the sun can trigger flares as well.
Conclusion:
In recent years treatments for systemic lupus erythematosus have improved significantly due to advances in medical technology and research into better understanding this complex condition. While there is still no cure for this autoimmune disorder yet available on the market today there are numerous options that can help reduce symptoms associated with it so those affected can live their lives without having to worry about flares up too often anymore!
At UnabridgedMD in rheumatology we offer specialized care for patients suffering from systemic lupus erythematosus (SLE), providing them with personalized treatment plans tailored towards their individual needs - something that traditional medical practices cannot always provide! If you're looking for a rheumatologist who understands your uniqueness and cares for you so that you can achieve disease remission to live to the life you are meant to live, then get in touch today!
Isabelle Amigues, MD, MS, RhMSUS
Email us at info@unabridgedmd.com
Call us at 3037314006
Keywords: `ANA, SLE, systemic Lupus, Lupus, discoid lupus, fever of unknown origin, elevated ESR, elevated CRP, arthritis, inflammatory arthritis, joint pain, joint swelling, best rheumatologist in Denver, Colorado








Comments